General Dentistry
Dental services for the whole family, from regular checkups to routine x-rays, fillings and extractions. At Cherwell Heights Dental Care we provide the highest level of dental care for all the family including consultations, regular dental health checks & x-rays and routine dental care such as filings & extractions.
Amalgam – or ‘silver fillings’
Dental amalgam is a common material used to fill cavities in teeth – but we do not use it in any form. Over the years, concerns have been raised about the use of amalgam because it contains mercury.
What is amalgam?
Amalgam is a combination of metals that has been the most popular and effective filling material used in dentistry for the last 150 years. While sometimes called ‘silver amalgam’, it actually consists of a combination of metals that include silver, mercury, tin and copper. Small amounts of zinc, indium or palladium also may be used. The compound aims to match the expansion and contraction of natural teeth as you sip hot or cold drinks.
Tooth-coloured materials now can be used to restore teeth so we do not use amalgam. However, the newer materials can’t be used for all situations – but we can advise you on the best course of treatment for you.
Call 01295 709 500 and we’ll guide you.
Nickel-Free Fillings
Allergy to nickel is rare but this is something we’d ask you on our patient history form when you join the practice. Some medical and dental products do contain nickel so while reaction to it is very rare there are a few things worth noting:
- Nickel has been used in dentistry for more than eighty years in both restorative work (fillings, crowns, bridges, partial dentures) and orthodontic appliances (wires, bands, brackets, and so on).
- Nickel is used in dentistry for several reasons. First, it makes a soft metal like gold harder. Secondly, combined with titanium, nickel becomes a shape-memory alloy used in orthodontics. Finally, nickel is inexpensive.
- The amount of nickel used in dental items can range from a few percent to over 50%.
- To limit exposure to nickel, let us know if you are nickel allergic.
- Wherever possible we confirm with the manufacturer of any dental appliances about any nickel used prior to use.
Reactions to orthodontics are rare, but if you are concerned about possible reactions from the use of nickel containing dental materials, just talk to us.
Call 01295 709 500 and we’ll guide you.
Extraction
Why this might be necessary?
If a tooth has been broken or damaged by decay, we will do our very best to repair it with a filling, crown or other dental treatment. But when there’s too much damage for the tooth to be repaired, the tooth may need to be extracted — or removed — from its socket in the bone. Moreover, a very loose tooth also will require extraction if it can’t be saved, even with bone replacement surgery (bone graft). There are other reasons that we may have to remove a tooth:
- Some people have extra teeth that block other teeth from coming through.
- Sometimes ‘baby teeth’ don’t fall out in time to allow the permanent teeth to come through.
- People getting braces may need teeth extracted to create room for the teeth that are being moved into place.
- Wisdom teeth, also called ‘third molars’, appear at the very back of each row of teeth, are often extracted either before or after they come through. They commonly appear during your late teens or early 20s. They need to be removed if they are decayed, cause pain or have a cyst or infection. These teeth can sometimes get stuck in the jaw (impacted) on their way through. This can irritate the gum, causing pain and swelling. In this case, the tooth must be removed. If you need all four wisdom teeth removed, they are all usually taken out at the same time.
There are a few more exceptional reasons to have the wisdom teeth removed:
- People receiving radiotherapy to the head and neck may need to have teeth in the field of radiation extracted.
- People receiving cancer drugs may develop infected teeth because these drugs weaken the immune system. Infected teeth may need to be extracted.
- Some teeth may need to be extracted if they could become a source of infection after an organ transplant. People with organ transplants have a high risk of infection because they must take drugs that decrease or suppress the immune system.
What will happen before an extraction?
We will take an X-ray of the area to help plan the best way to remove the tooth. We will ask you about your full medical and dental history and a list of all medicines you take. This should include prescription and over-the-counter medicines, vitamins and supplements.
If you are having wisdom teeth removed, you may have a panoramic X-ray. This X-ray takes a picture of all of your teeth at once. It can show several things that help to guide an extraction:
- The relationship of your wisdom teeth to your other teeth
- The upper teeth’s relationship to your sinuses – those hollow cavities behind your cheekbones and forehead
- The lower teeth’s relationship to a nerve in the jawbone that gives feeling to your lower jaw, lower teeth, lower lip and chin. This nerve is called the inferior alveolar nerve.
- Any infections, tumours or bone disease that may be present.
Depending on your situation, we may prescribe antibiotics to be taken before and after extraction. Antibiotics are more likely to be given if you:
- have infection at the time of surgery
- have a weakened immune system
- will have a long surgery
- have specific medical conditions
You may have intravenous (IV) anaesthesia, which can range from conscious sedation to general anaesthesia. If so, we will give you clear instructions to follow. You should wear clothing with short sleeves or sleeves that can be rolled up easily. This allows access for an IV line to be placed in a vein. We advise you not to eat or drink anything for six or eight hours before the procedure.
If you have a cough, stuffy nose or cold up to a week before the surgery, let us know. We may want to avoid anaesthesia until you are over the cold. If you had nausea and vomiting the night before the procedure, call us first thing in the morning (01295 709 500). We may need to change your planned anaesthesia or the extraction may have to be rescheduled.
Do not smoke on the day of surgery. This can increase the risk of a painful problem called ‘dry socket’ (see below).
After the extraction, it is often a good idea to have someone to drive you home and stay there with you. We will give you post-surgery instructions. It is very important that you follow them.
How do you do an extraction?
There are two types of extractions:
- A simple extraction is performed on a tooth that can be seen in the mouth. In a simple extraction, we loosen the tooth with an instrument called an elevator. Then we use an instrument called forceps to remove the tooth.
- A surgical extraction is a more complex procedure. It is used if a tooth may have broken off at the gum line or has not come into the mouth yet. We make a small incision (cut) into your gum. Sometimes it’s necessary to remove some of the bone around the tooth or to cut the tooth in half in order to extract it – but all this is under appropriate anaesthetic!
Most simple extractions can be done using just an injection (a local anaesthetic). If you need it, we can provide medicines to help you relax.
For a surgical extraction, you will receive a local anaesthetic, or you may also have anaesthesia through a vein (intravenous). Some people may need general anaesthesia – and we can discuss which option best suits your needs
If you are receiving conscious sedation, you may be given steroids as well as other medicines in your IV line. The steroids help to reduce swelling and keep you pain-free after the procedure.
During a tooth extraction, you can expect to feel pressure, but no pain. Remember – we give ‘dentistry with a gentle touch’.
What happens afterwards?
We will give you detailed instructions on what to do and what to expect after your surgery. If you have any questions, make sure to ask us anything that concerns you while you are with us.
Having a tooth taken out is ‘surgery’ but this shouldn’t be taken as dramatic as having your appendix removed!
Naturally enough, you can expect some discomfort after even simple extractions. Usually it is mild. Research has shown that taking nonsteroidal anti-inflammatory drugs (NSAIDs) can greatly decrease pain after a tooth extraction. These drugs include ibuprofen, such as Neurofen® and others. As a general rule, follow the patient instruction leaflet although we will also give you a clear guide at the time.
Surgical extractions generally cause more pain after the procedure than simple extractions. The level of discomfort and how long it lasts will depend on how difficult it was to remove the tooth. We may prescribe pain medicine for a few days and then suggest an NSAID. Most discomfort disappears after a couple of days.
Again, we will give you very specific help and guidance that is right for you.
What are the risks?
A problem called a ‘dry socket’ develops in about 3% to 4% of all extractions. This occurs when a blood clot doesn’t form in the hole or the blood clot breaks off or breaks down too early.
In a dry socket, the underlying bone is exposed to air and food. This can be very painful and can cause a bad odour or taste. Typically dry sockets begin to cause pain the third day after surgery.
Dry socket occurs up to 30% of the time when impacted teeth are removed. It is also more likely after difficult extractions. Smokers and women who take birth control pills are more likely to have a dry socket. Smoking on the day of surgery further increases the risk. A dry socket needs to be treated with a medicated dressing to stop the pain and encourage the area to heal.
Infection can set in after an extraction. However, you probably won’t get an infection if you have a healthy immune system.
As always, we will address all your concerns and anxieties with a sympathetic ear and give you specific advice at the time
So, if you are new to the area, have a particular concern, or are in any way anxious – you are very welcome to come on in and talk to us.
Call 01295 709 500 – we are here to help you.
Family Dentistry
As parents ourselves, we know no parent wants to see their child suffering with an abscess or painful tooth cavity – so early years’ experience at the dentist is crucial to instil confidence and trust in getting regular dental support in later years.
Fortunately, recent advances in dentistry have allowed us to identify decay risks early and follow this with procedures designed to heal these areas before they need fillings.
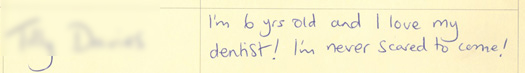
While we are a private practice for adults, patient’s children under 16 are treated with our same high level of care and attention but under National Health Service funding – if you have a particular concern about your child’s teeth or if they have any anxiety, please give us a call 01295 709 500 – we are here to help you.


